Tinea pedis in Adult
See also in: Cellulitis DDxAlerts and Notices
Important News & Links
Synopsis

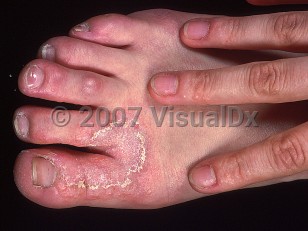
Tinea pedis (athlete's foot) is a localized superficial fungal infection of the foot. Trichophyton rubrum, Trichophyton mentagrophytes, and Epidermophyton floccosum are the dermatophytes responsible for most cases of tinea pedis.
Occlusive footwear with increased local humidity, as well as use of communal pools or baths, predisposes to tinea pedis. Athletes are at increased risk (ie, "athlete's foot"). Secondary (gram-negative) bacterial infection, especially in diabetic patients, may occur. Tinea pedis is more common in men. There is no ethnic predilection, and the prevalence increases with age.
The clinical presentation of tinea pedis may vary. The web spaces and soles are affected most frequently, but the condition may spread to involve the nonplantar surfaces of the foot as well. Interdigital maceration, especially of the lateral toe webs, is commonly seen. Tinea pedis is frequently asymmetric with one foot only being affected or disease being more widespread on one foot than the other. The degree of associated pruritus varies, but most cases are asymptomatic. Trichophyton rubrum may present with a red, scaly, moccasin-like plaque involving the sole. The bullous form of tinea pedis is usually caused by Trichophyton interdigitale (formerly T mentagrophytes var interdigitale). Onychomycosis may be associated.
Interdigital cracking and maceration may act as a portal of entry for pathogens and may predispose to lymphangitis or cellulitis. A dermatophytid reaction (also called an "id reaction") is a hypersensitivity process that can occur secondary to tinea pedis. The condition manifests on the lateral aspects of the fingers and may mimic dyshidrotic dermatitis. This hypersensitivity process will resolve with adequate treatment of the dermatophyte infection.
Immunocompromised patient considerations: In patients with human immunodeficiency virus (HIV) infection and other T-cell disorders, interdigital tinea pedis has been noted to spread to involve the dorsal foot in an extensive manner.
Occlusive footwear with increased local humidity, as well as use of communal pools or baths, predisposes to tinea pedis. Athletes are at increased risk (ie, "athlete's foot"). Secondary (gram-negative) bacterial infection, especially in diabetic patients, may occur. Tinea pedis is more common in men. There is no ethnic predilection, and the prevalence increases with age.
The clinical presentation of tinea pedis may vary. The web spaces and soles are affected most frequently, but the condition may spread to involve the nonplantar surfaces of the foot as well. Interdigital maceration, especially of the lateral toe webs, is commonly seen. Tinea pedis is frequently asymmetric with one foot only being affected or disease being more widespread on one foot than the other. The degree of associated pruritus varies, but most cases are asymptomatic. Trichophyton rubrum may present with a red, scaly, moccasin-like plaque involving the sole. The bullous form of tinea pedis is usually caused by Trichophyton interdigitale (formerly T mentagrophytes var interdigitale). Onychomycosis may be associated.
Interdigital cracking and maceration may act as a portal of entry for pathogens and may predispose to lymphangitis or cellulitis. A dermatophytid reaction (also called an "id reaction") is a hypersensitivity process that can occur secondary to tinea pedis. The condition manifests on the lateral aspects of the fingers and may mimic dyshidrotic dermatitis. This hypersensitivity process will resolve with adequate treatment of the dermatophyte infection.
Immunocompromised patient considerations: In patients with human immunodeficiency virus (HIV) infection and other T-cell disorders, interdigital tinea pedis has been noted to spread to involve the dorsal foot in an extensive manner.
Codes
ICD10CM:
B35.3 – Tinea pedis
SNOMEDCT:
6020002 – Tinea pedis
B35.3 – Tinea pedis
SNOMEDCT:
6020002 – Tinea pedis
Look For
Subscription Required
Diagnostic Pearls
Subscription Required
Differential Diagnosis & Pitfalls

To perform a comparison, select diagnoses from the classic differential
Subscription Required
Best Tests
Subscription Required
Management Pearls
Subscription Required
Therapy
Subscription Required
References
Subscription Required
Last Reviewed:08/15/2019
Last Updated:12/09/2020
Last Updated:12/09/2020
 Patient Information for Tinea pedis in Adult
Patient Information for Tinea pedis in Adult
Premium Feature
VisualDx Patient Handouts
Available in the Elite package
- Improve treatment compliance
- Reduce after-hours questions
- Increase patient engagement and satisfaction
- Written in clear, easy-to-understand language. No confusing jargon.
- Available in English and Spanish
- Print out or email directly to your patient
Upgrade Today

Tinea pedis in Adult
See also in: Cellulitis DDx